Introduction: Our aim was to assess clinical and histologic characteristics of intestinal failure associated liver disease (IFALD) in children.
Methods: This was a retrospective single center study. In total, 89 consecutive children with intestinal failure (IF) and liver biopsy obtained between years 2006-2018 were included. Liver biopsies were analyzed for histology with simultaneous measurements of serum liver biochemistry, citrulline, spleen size and cholelithiasis (ultrasound, n=86). Presence of esophageal varices was based on gastroscopy (n=70). Fisher’s exact and Mann Whitney U test were used for comparisons.
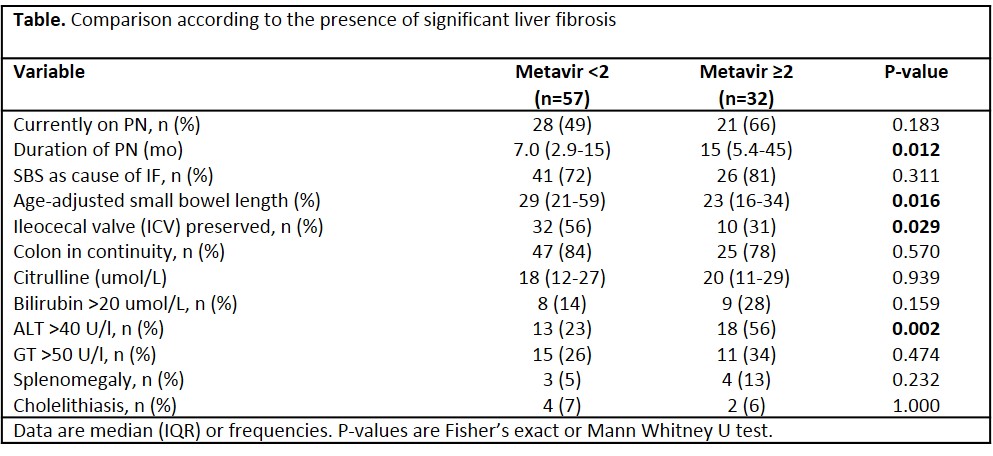
Results: Median patient age was 3.1 years (IQR 0.6-9.3), age-adjusted small bowel length was 26% (17-48%) and 49 patients were currently receiving PN at the time of liver biopsy. The causes of IF included short bowel syndrome (SBS, n=67), primary motility disorders (n=20) and enteropathies (n=2). Significant histologic liver fibrosis (Metavir stage ≥2), cholestasis, portal inflammation and steatosis was observed in 36%, 29%, 26% and 31% of patients. Any degree of cholestasis (49% vs 5%), portal inflammation (43% vs 5%) and fibrosis (65% vs 38%) were more frequent during PN (P<0.05 for all), whereas steatosis (30% vs 29%, P=NS) and significant fibrosis were equally common after weaning off PN (Table). Splenomegaly was observed in seven (8%) and esophageal varices in one (1.4%) patient, mostly during PN delivery. Cholelithiasis was observed in six (7%) patients. Presence of significant liver fibrosis associated with short remaining small intestine, prolonged PN, missing ileocecal region and elevated ALT (Table). One patient died of IFALD and one with associated extrahepatic portal vein occlusion underwent liver transplantation after weaning off PN.
Conclusion: Cholestasis and portal inflammation are nearly exclusively associated with PN delivery, whereas significant fibrosis and steatosis frequently persist after weaning off PN. Splenomegaly and esophageal varices were infrequent complications of pediatric IFALD. Although IFALD was uncommon cause of death or liver replacement therapy, long-term significance of persisting fibrosis and steatosis needs to be resolved.
.jpg )