Introduction: Endoscopic surveillance of the transplanted intestine is essential for early diagnosis and successful management of graft rejection. End ileostomies are easy to survey, but patients often have high output leading to renal impairment and electrolyte disturbance. Increasingly colon inclusion has become standard of care but endoscopy via an end colostomy can be difficult and lead to failure to access the terminal ileum. In addition a standard loop ileostomy proximal to a transplanted colon does not take advantage of the fluid balance advantages conferred by colon inclusion. In 2017, we started to use a Bishop Koop anastomosis proximal to an anastomosis between transplanted and native colon.
Methods: This is a retrospective review of a prospectively held database of all intestinal-containing grafts from 2017.
Results: Since 2017, 10/20 transplants have included a Bishop-Koop stoma. In the 10 patients who did not have Bishop Koop stomas this was as a consequence of either concerns regarding the native colon at transplant (2 patients) or recipient pathology that rendered distal continuity inappropriate or technically impossible (pan proctocolectomy, ileal pouch).
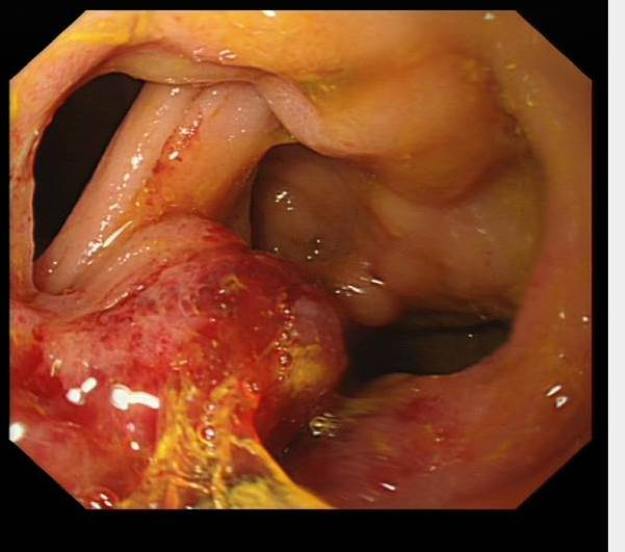
Endoscopic surveillance was quicker and more comfortable for patients and ileal visualisation was possible in all cases. Two patients have subsequently undergone stoma reversal and this has proven technically easier than with our previous stoma.
Conclusion: We describe the use of a Bishop Koop stoma for patients undergoing intestinal transplantation. This has resulted in improved endoscopic surveillance, fluid balance and patient satisfaction compared to our previous use of end colostomies. Stoma reversal with the Bishop Koop is a simpler undertaking.
.jpg )