Introduction: Post-transplant lymphoproliferative disorder (PTLD) is one of the most serious complications that can develop after a transplant and rates are reported to be highest in intestinal and multivisceral transplants. This study looks at the risk of developing PTLD with different Epstein-Barr virus (EBV) serostatus in donor and recipient.
Methods: This is a retrospective observation study of case notes. Key data collected includes EBV status in the donor and recipient prior to transplant, time to development of PTLD, histology specimen reports and mortality outcomes.
Results: The intestinal and multivisceral transplant service at Addenbrooke’s Hospital, Cambridge, UK transplanted 80 patients from 2000-2018. There were 12 cases which developed PTLD giving a rate of developing PTLD of 15% in our cohort and mortality of 16.7%. Histology was obtained in 11 cases with one case having an inaccessible lymph node but characteristic features of PTLD. The histology specimens showed 100% stained positive for EBV, whilst 66.7% were lymphomas and 33.3% were pre-lymphomas. The development of PTLD occurred within 3 months in 66% of cases, 3-6 months in 17% of cases, and 12-18 months in 17% of cases.
Information on donor and recipient EBV serostatus was available in 44 consecutive patients, which included 10 of the 12 cases of PTLD. 20 patients developed persistent EBV viraemia, and 10 of these patients developed PTLD, taking approximately 2 weeks to progress.
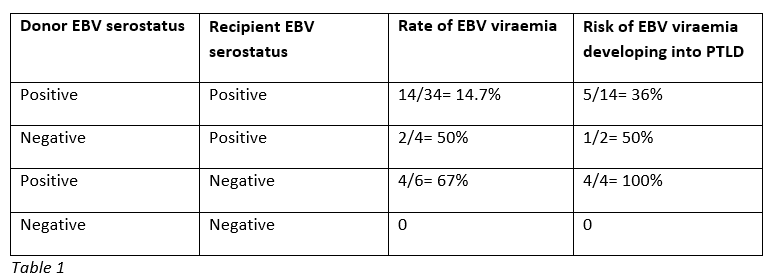
The risk of persistent EBV viraemia developing with different donor and recipient EBV serostatus and subsequent risk of developing PTLD is shown below in table 1.
The risk of PTLD developing in groups with different donor and recipient EBV serostatus is shown below in table 2.
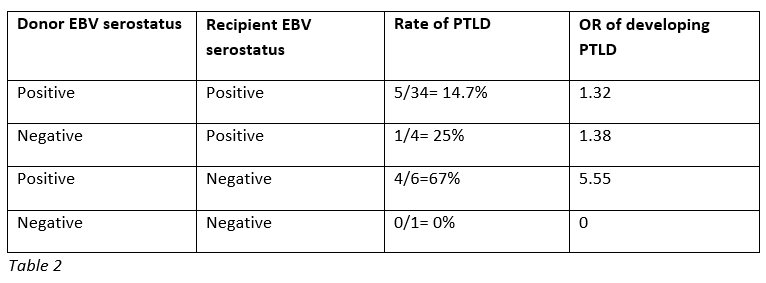
Conclusion: The key finding of this study is that when an EBV seronegative recipient receives and intestinal graft from an EBV seropositive donor, there is 67% risk of developing EBV viraemia and in this group 100% will develop PTLD. Furthermore, the two deaths directly attributable to PTLD occurred in this group, suggesting that primary infection has a more serious disease course. Taken together, this gives a strong argument for matching EBV serostatus, particularly for recipients who are EBV negative. In circumstances where this is not possible, for example a super-urgent listing due to graft failure or a highly sensitised recipient, a persistent EBV viraemia should be treated early and effectively to stop progression to PTLD.
.jpg )