Introduction: Acute rejection (AR) remains a major determinant of morbidity and mortality after ITX. We studied patterns of AR and graft loss to understand potential loci for intervention.
Methods: We reviewed all ITX without concomitant liver graft between 2011 and 2018 at a single-center using a prospectively maintained database. AR, patient and graft survival were outcomes of interest.
Results: We analyzed 72 ITX without liver replacement. Twenty-eight grafts had at least one episode of AR (39%). Majority of AR occurred during first 6 months (57%) post- ITX and remainder occurred sporadically during the entire post-ITX period. Of 35 total episodes of AR among 28 grafts, 13 were mild (37%), 4 moderate, (11%), and 18 (51%) severe AR based on histological grades. Patient survival did not show a difference between ITX with and without AR (p=0.750), though, AR was the most common cause of mortality (n=6, 8%). Censoring death with functioning graft (n=12), AR was the most common cause of graft loss (n=11, 15%). Mild AR tended to develop early (< 12 months) post-ITX. Severe AR was observed evenly during the entire post-ITX period (Figure 1).
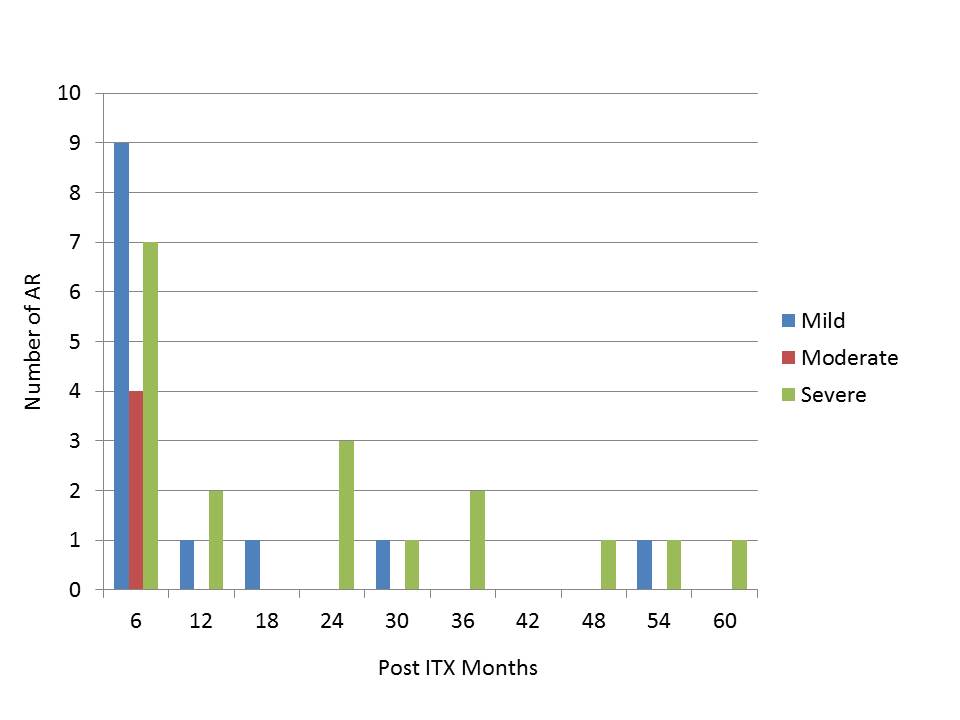
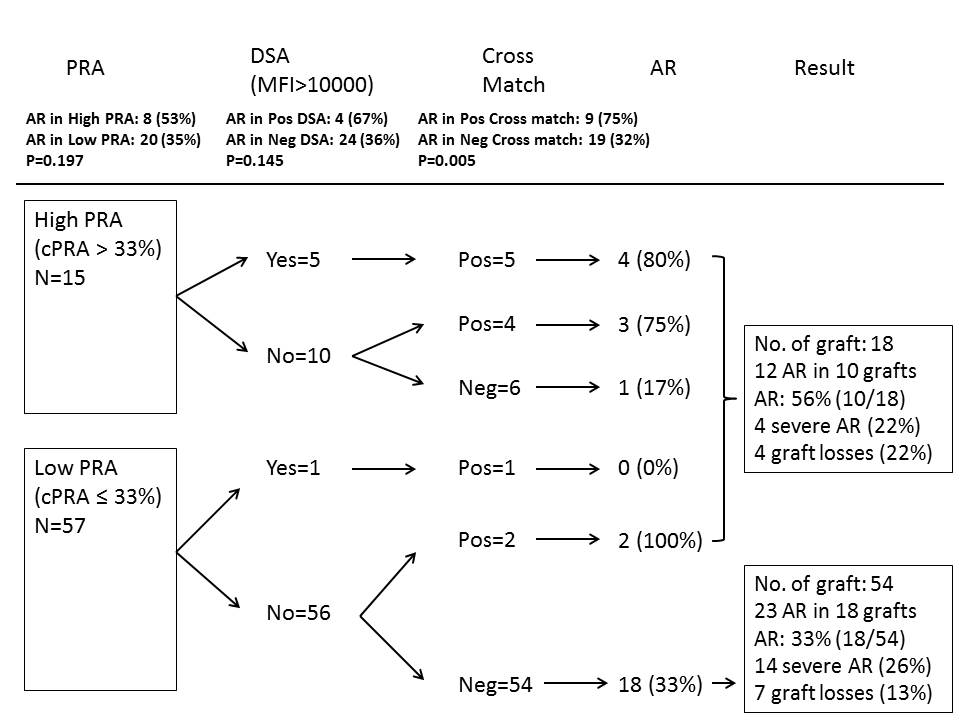
Conclusion: Our analysis supports previous reports that severe AR is a major cause for graft loss and mortality in ITX. Presence of PRA, DSA and a positive cross match seem related to risk of developing AR. Of note, patients with no apparent heighted immunological risk factors also develop severe AR with a high frequency of graft loss. Mild to moderate AR has no apparent impact on outcome.
.jpg )