Introduction: With improved survival of children with intestinal failure (IF), it is important to explore the subsequent impact on long-term physical function. This study evaluates functional outcomes of muscle strength, fatigue and physical activity (PA) and identifies clinical factors that may be predictive of impairment.
Methods: Cross-sectional study in children with IF on long term parenteral nutrition (PN) compared to healthy age and gender matched controls (HC’s). Assessments included: Bruininks-Oseretsky Test of Motor Proficiency-2 (Strength and Agility subtest) (BOT-2), Grip strength, Paediatric Quality of Life (PedsQL) Physical Function subscale and Multi-Dimensional Fatigue Module, and Benefits/Barriers to PA Questionnaire. PA was measured using an accelerometer. Medical data was collected by chart abstraction.
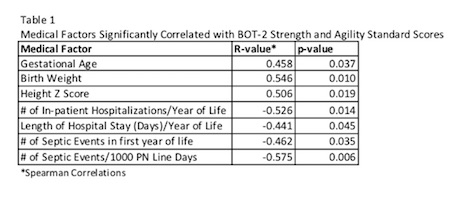
Results: Participants included 21 children with IF (14 male) at a median age of 8.33 (IQR 6.96, 11.04) years and 33 HC’s (20 males), 8.25 (6.67, 10.79) years. In those with IF, 13 (62%) were born prematurely (gestational age 35 (33, 38.5) weeks) and the most common diagnosis was gastroschisis (38%). Children received PN for 14 (11, 16) hours/day, with 17 (81%) dependent since infancy. Since birth, there was a median of 4 (1, 9) septic episodes and 15 (7.5, 24.5) in-patient hospitalizations. Mean BOT-2 standard scores [population norm of 50, SD of 10] were 61.27 +/- 6.8 for HC’s and 45.67 +/- 9.1 for children with IF, with 6/21 (28%) below average (>1SD below mean). 13/21 (62%) children fell >1SD below the mean norm for grip strength, compared to only 6/33 (18.2%) HC’s. Mean steps/day in children with IF was 9842 +/- 4077 compared to HC’s with 13104 +/- 5416. There was a significant difference between groups in strength and agility (p<.001), grip strength (p=.001), and total steps/day (p=.047). Medical variables significantly associated with BOT-2 scores are shown in Table 1.
Results of the PedsQL are shown in Figure 1.
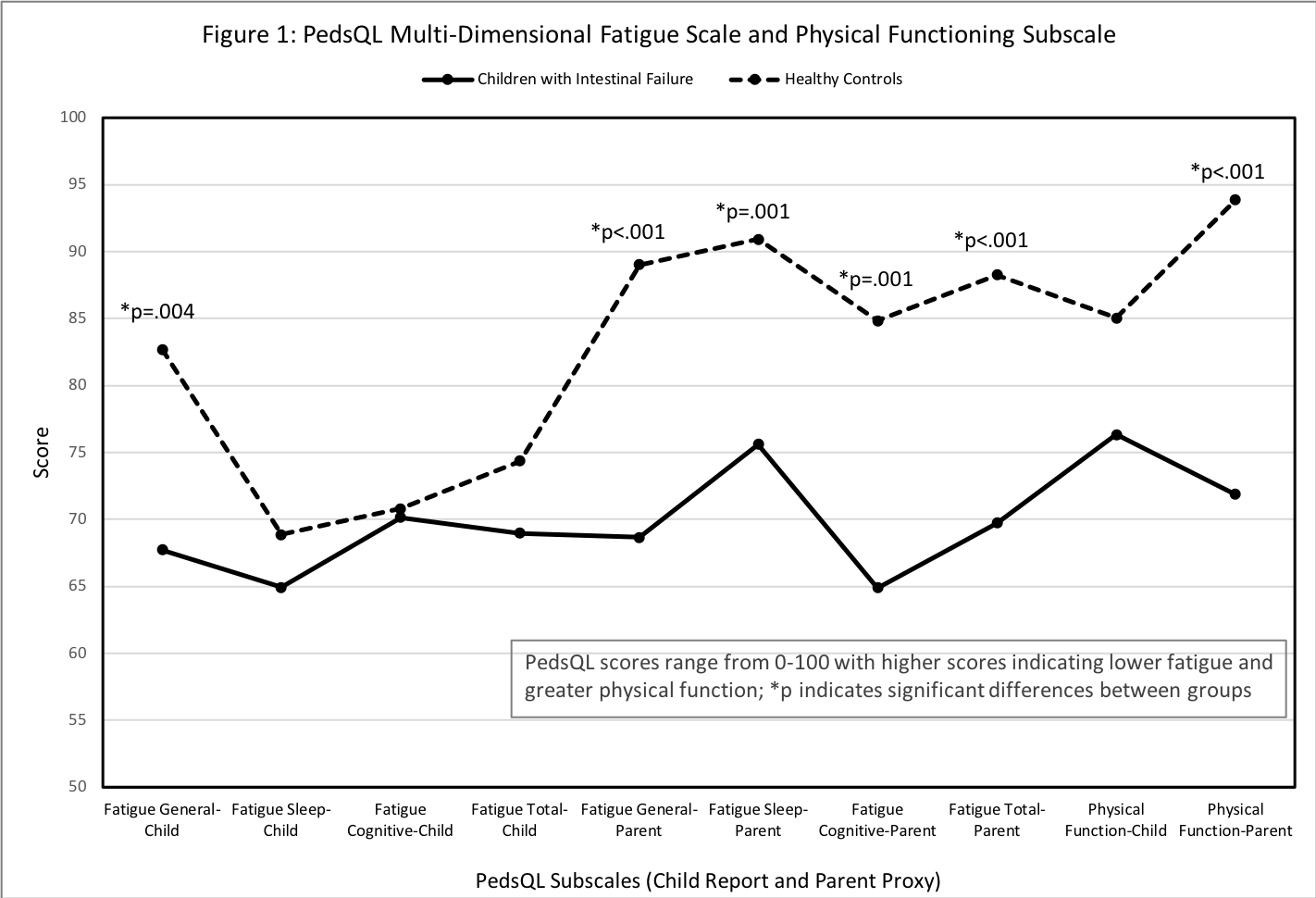
Parents report greater fatigue (r=-.538, p=.012) and poorer physical function (r=-.650, p=.001) in children with more hospitalizations. Barriers to PA in children with IF included “I am tired” and “I am worried about my line.”
Conclusion: Factors such as prematurity, decreased linear growth, hospitalization and septic events may have a significant impact on physical function outcomes in children with IF on PN. Ongoing development of medical and rehabilitation intervention strategies is vital to optimize outcomes.
.jpg )