Introduction: Intestinal transplantation (ITx) can be a successful procedure for select candidates with intestinal failure (IF). However, there is limited data on variables and characteristics that predict successful outcome. The aim of this study was to analyze a large dataset to determine outcome predictors.
Methods: An IRB approved, prospective database has been maintained since the inception of the program in 1991. Patient inclusion was closed in December 2018. All recipients of intestinal grafts were included. Multiple pre-, peri, and post-transplant variables (n = 35) were collected and included in the analysis. The end point was 1-year patient and graft survival. Standard statistical analysis was undertaken.
Results: 128 patients underwent 151 ITx including 35 isolated intestine (I-ITx), 77 liver-intestine (OLT-SBT), 29 multivisceral (MVT) and 11 modified multivisceral (MMVT).
58% were male, 78% were children, and 77% had surgical IF etiologies. At ITx, the median MELD/PELD at ITx was 34 with 43% hospitalized.
The majority of patients received induction immunotherapy with either interleukin-2 receptor antagonist [IL2RA] (58%) or antibody induction with rabbit antithymocyte globulin [rATG] / OKT3 (34%).
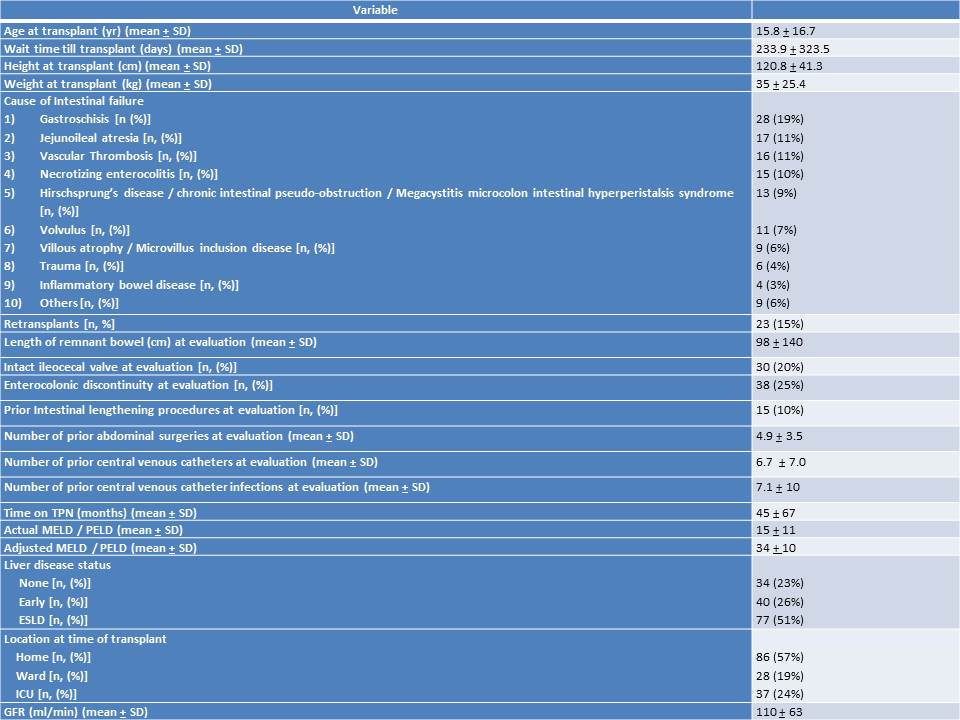
Relevant patient clinical characteristics are summarized in the table below:
Significant predictors for improved graft survival were:
Recipient weight (<20 kg), age group (pediatrics), graft type (liver inclusive intestinal graft), panel reactive antibody < 20%, absence of donor specific antibodies, negative crossmatch, warm ischemia time < 1 hr, use of induction immunosuppression, ventilator time < 7 days, length of stay < 80 days, and transplant era (2001-2018).
Significant predictors for improved patient survival were:
Cold ischemia time < 10 hrs, warm ischemia time < 1 hr, absence of recipient splenectomy, use of induction immunosuppression, length of stay < 80 days, and transplant era (2001-2018).
The patient and graft survival at 1-year was 82% and 69%.
Conclusion: The results of ITx have improved over time. Several perioperative factors were identified that impact early outcome. Especially important for graft survival are variables that can be altered including donor: recipient match, preformed donor specific antibodies, ischemia times, and immunosuppression. Further investigations are required to improve ITx outcomes.
.jpg )