Introduction: Management of intestinal failure secondary to LSHD is based on parenteral nutrition (PN) associated to proximal jejunostomy. Early prophylactic subtotal enterectomy (SE) is not recommended since the excluded intestine allows growth of the abdominal cavity, which may be needed to host a graft in case of intestinal transplantation. This study evaluates the risk of enterocolitis linked to the excluded bowel in such patients.
Methods: The charts of all patients with LSHD requiring PN and enterostomies, managed from 1986 to 2017 in our institution, were reviewed. Subtotal enterectomy was performed, in our center, only after occurrence of complications due to the excluded bowel. Two patients underwent a subtotal enterectomy during the initial management and before referral to our center. They were excluded from this study.
Results: Twenty seven patients were included.
Initial management resulted in totally diverting jejunostomy in 26 patients and a loop jejunostomy in one (median length from duodeno-jejunal flexure to stoma 30 cm [0-90 cm]).
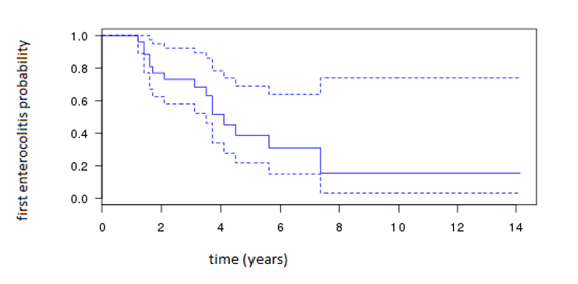
Sixteen patients (59.2%) presented at least one episode of enterocolitis (EC). Median age at first EC was 2.2 years [0.3- 7.1]. Fifteen underwent a subtotal enterectomy (4 as an emergency procedure for). Median age at SE was 3.1 years [1.3- 7.4].
Three patients underwent a longitudinal seromyotomy with transfer of the jejunostomy downstream at initial management for one and at the time of subtotal enterectomy for two (9 months and 4 years).
13 patients underwent transplantation later (7 liver+ intestinal and 6 intestinal).
Conclusion: Patients with LSHD carry a high risk of early complications linked to the excluded bowel. Since there is a paradigm shift regarding the indications of intestinal transplantation in patients with intestinal failure, these data represent a first step to better evaluate the benefice / risk balance of preserving the excluded bowel for growth of the abdomen in view of eventual intestinal transplantation. Furthermore, the risks of repeated sepsis on long term liver function should also be assessed in order to discuss more rationally the better timing of enterectomy in this population having already PN and its associated risk of liver disease.
.jpg )