Introduction: Patients (pts) with short bowel syndrome (SBS) have high morbidity and mortality mainly related to their residual intestinal anatomy/function and clinical status. Better outcomes are achieved when this condition is managed at a comprehensive multidisciplinary unit.
Aim: To analyze long-term results and chances of achieving Intestinal Sufficiency (IS) of all children with SBS referred to a comprehensive Intestinal Failure, Rehabilitation and Transplant Unit from 3/2006 to 12/2018
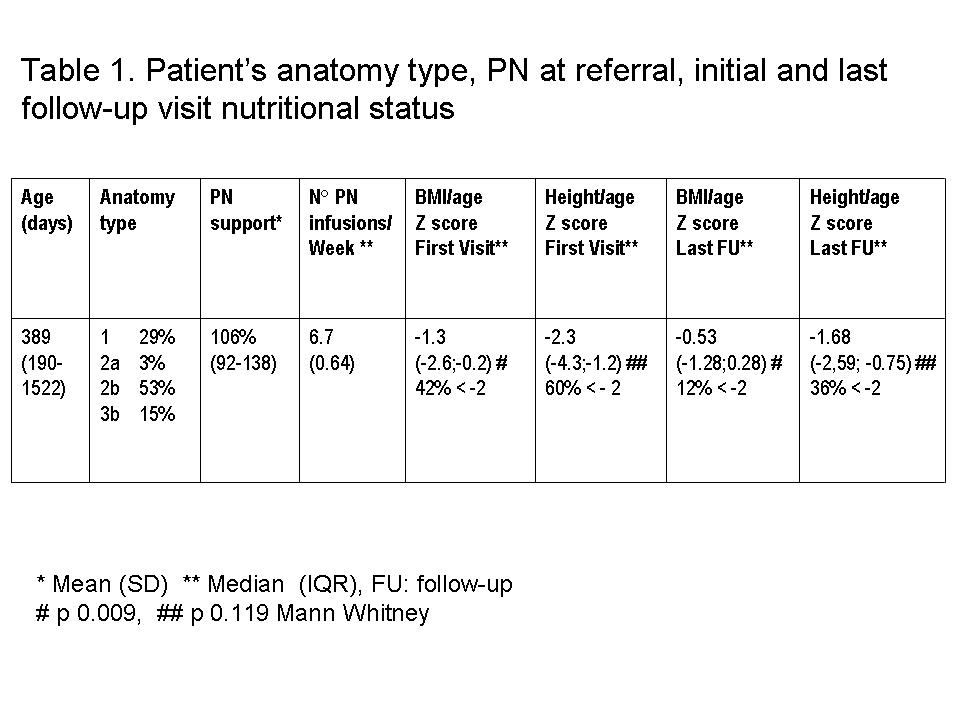
Material and methods: This is a retrospective review of a prospectively filled database, including pediatric pts with SBS .Demographic data, diagnosis, nutritional status, parenteral nutrition (PN) support, as % of the basal metabolic rate (no protein Kcal), intestinal anatomy type (1 -terminal jejunostomy-; 2 -jejuno colonic anastomosis; 3 -jejuno-ileo colonic anastomosis; subtypes by length: A< 40 cm and B > 40 cm; treatment implemented [Groups: PN+MR (PN + Medical Rehabilitation); SR+MR (Surgical + Medical Rehabilitation) and ITx (Intestinal Transplantation)]. were analyzed on SPSS.
Results: 62 pts with SBS out of 102 pts with chronic intestinal failure admitted in our program, were analyzed. 41 were male, 25 premature, 48 with neonatal SBS. Etiology of SBS included: gastroschisis (15), intestinal atresia (11), Hirschprung (10), NEC (10), post natal volvulus (7) and perinatal volvulus (4).
Pts´ anatomy type, PN at referral, initial and last follow-up visit nutritional status, are shown in Table 1. Median (IQR) time on PN before referral 0.62 (0.25-2.2) years. Figure 1 shows treatment implemented and outcomes. In the long term 30 (48.4%) pts were able to achieve IS; 25 % of the pts of the PN+MR group, Median IQR 1.2 (1-2.4) years since PN initiation (sPNi); 69% of the SR+MR group Median (IQR) 5.3 (1.4-8.9) years sPNi; and 76% of the ITx group (Median (IQR): 7 (2.5-10.8) sPNi, (PN+MR vs SR+MR and ITx: p= 0.004). From the ITx group, 5 pts failed in the long-term, re-starting PN, 2 died. Other 2 ITx pts died with IS. The overall 1, 5 and 10-year survival sPNi: 97%, 65.4% and 61.2% respectively, independently of the treatment implemented.
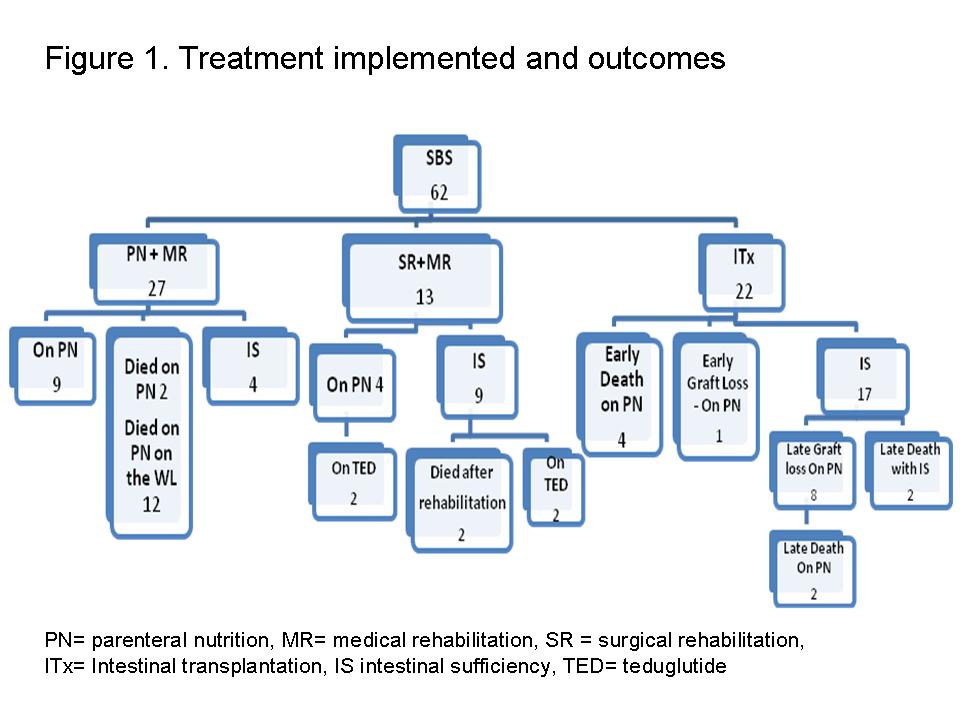
Conclusions: Although IS could be achieved under each line of therapy group, SR+MR allowed higher rate of IS with long term maintenance; ITx had higher chances of achieving IS, but there is drop out in the long term. Long-term survival of pts with SBS can be achieved when they are managed under a comprehensive program.
.jpg )