Background: Balancing immunosuppression to control rejection and prevent infection is critical to optimize patient and graft survivals after intestinal transplantation (ITx). We previously demonstrated that >4% peak donor T-cell chimerism in blood (macrochimerism) is associated with reduced graft rejection, DSA development and slower recipient T cell repopulation in the graft. We hypothesize that the absence of blood macrochimerism and faster recipient T-cell replacement in the graft may be used as biomarkers to predict impending rejection.
Methods: Serial surveillance intestinal biopsies were performed at regular intervals following transplant. T-cell chimerism was assessed from peripheral blood and ileal graft tissue with multicolor flow cytometry using donor- and recipient-specific HLA antibodies.
Result: 11 multivisceral transplant (MVTx), 1 liver-intestine transplant (LITx) and 9 isolated ITX (iITx) recipients were included. Patients and grafts were ABO compatible and randomly paired for HLA without crossmatch. Patients received immunosuppression induction with antithymocyte globulin and steroids, followed by lifelong tacrolimus-based maintenance therapy. One and three-year patient survival was 90.5% and 74%, respectively. T-cell macrochimerism developed in 14 recipients, peaked within 48 days and persisted for as long as 378 days (median 150 days). Patients with macrochimerism had a significantly greater moderate to severe rejection-free survival (p=0.001) and overall graft survival (p=0.016). Macrochimerism was detected more commonly in MVTx recipients (10/11 MVTx, 0/1 LITx and 4/9 iITx), and was associated with reduced de novo Class I (p=0.0003) and II (p=0.0038) DSA development (Fig. 1). Early postoperative recipient T-cell replacement >5% in the lamina propria of the ileal graft was associated with subsequent rejection (p=0.00047) in patients without macrochimerism (Fig. 2) and remained elevated following resolution of rejection. When macrochimerism is present and the donor is greater than 1 year of age, early recipient replacement of lamina propria T cells >5% may indicate imminent rejection. In donors less than 1 year of age however, rapid recipient replacement of the graft mucosa cell population is frequently seen without rejection.
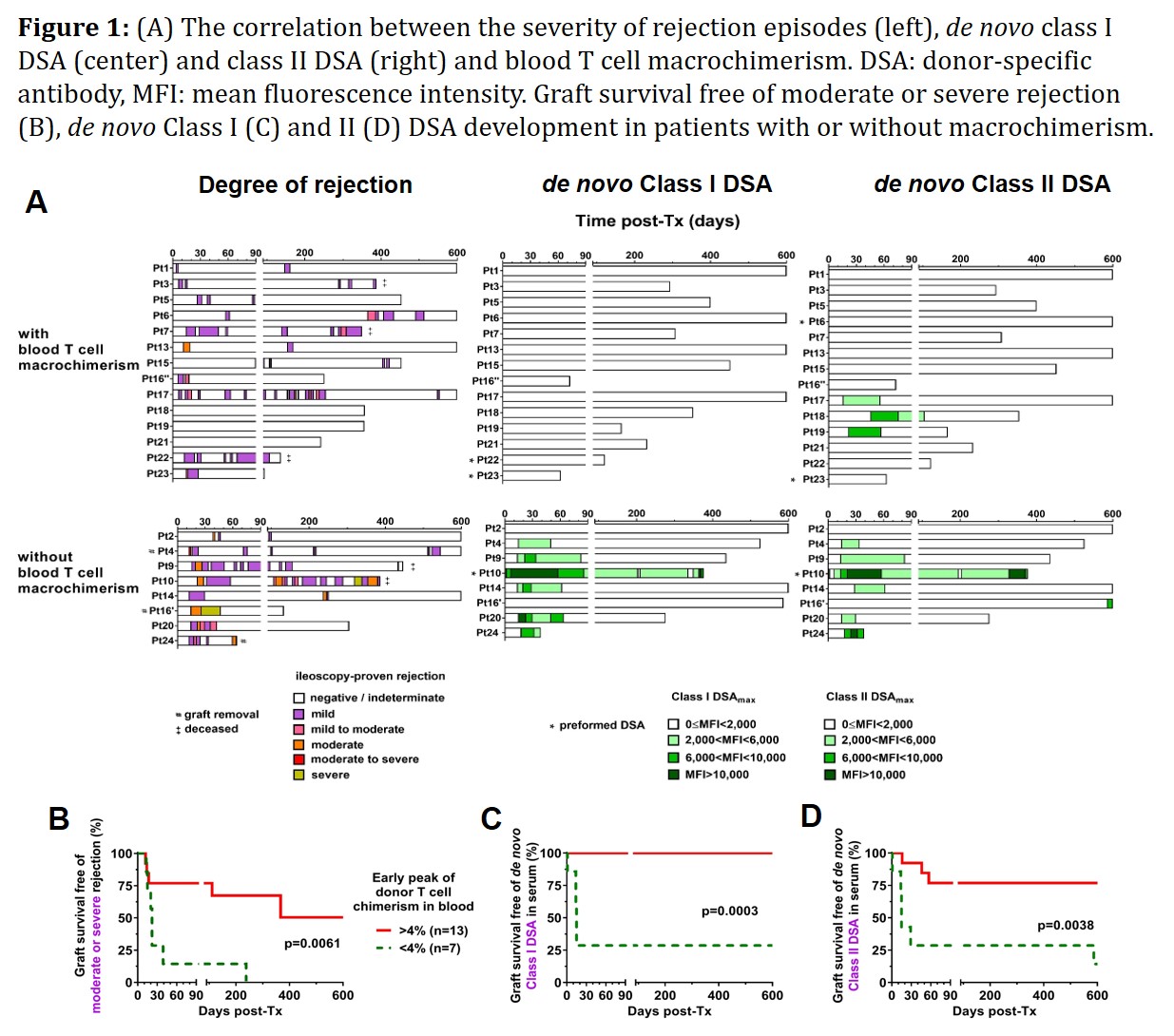
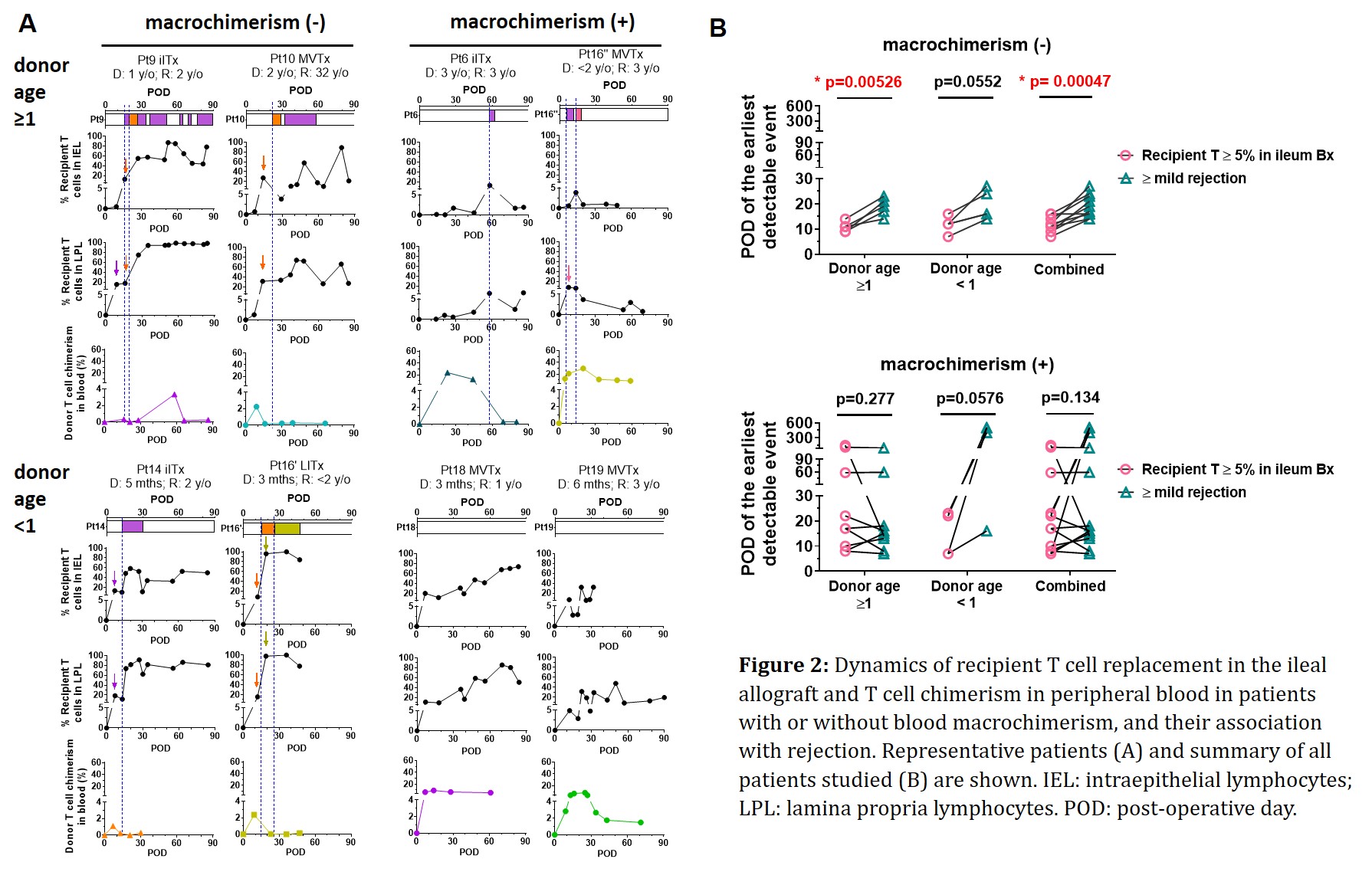
Conclusions: Peripheral T-cell macrochimerism and early recipient T-cell replacement in the graft could serve as potential biomarkers for guiding personalized immunosuppression in intestinal transplant patients.
.jpg )