Introduction: Although intestinal failure (IF) patients cared in expert centers have good long-term outcomes, acute mesenteric ischemia (AMI) is known as an independent risk factor of an impaired prognosis and is still considered a hopeless condition by many physicians. The aim of this study was to investigate the long-term outcomes of survivors from bowel resection for AMI.
Methods: Retrospective cohort study of consecutive patients referred to a tertiary care IF unit from 2006 and 2015 after bowel resection for AMI. Patients with ongoing or non-surgical AMI were not included. Cox regression analyses assessed predictors of parenteral support (PS) independence and AMI recurrence. Results are shown as Hazard Ratios (HR) and 95% Confidence Interval (CI).
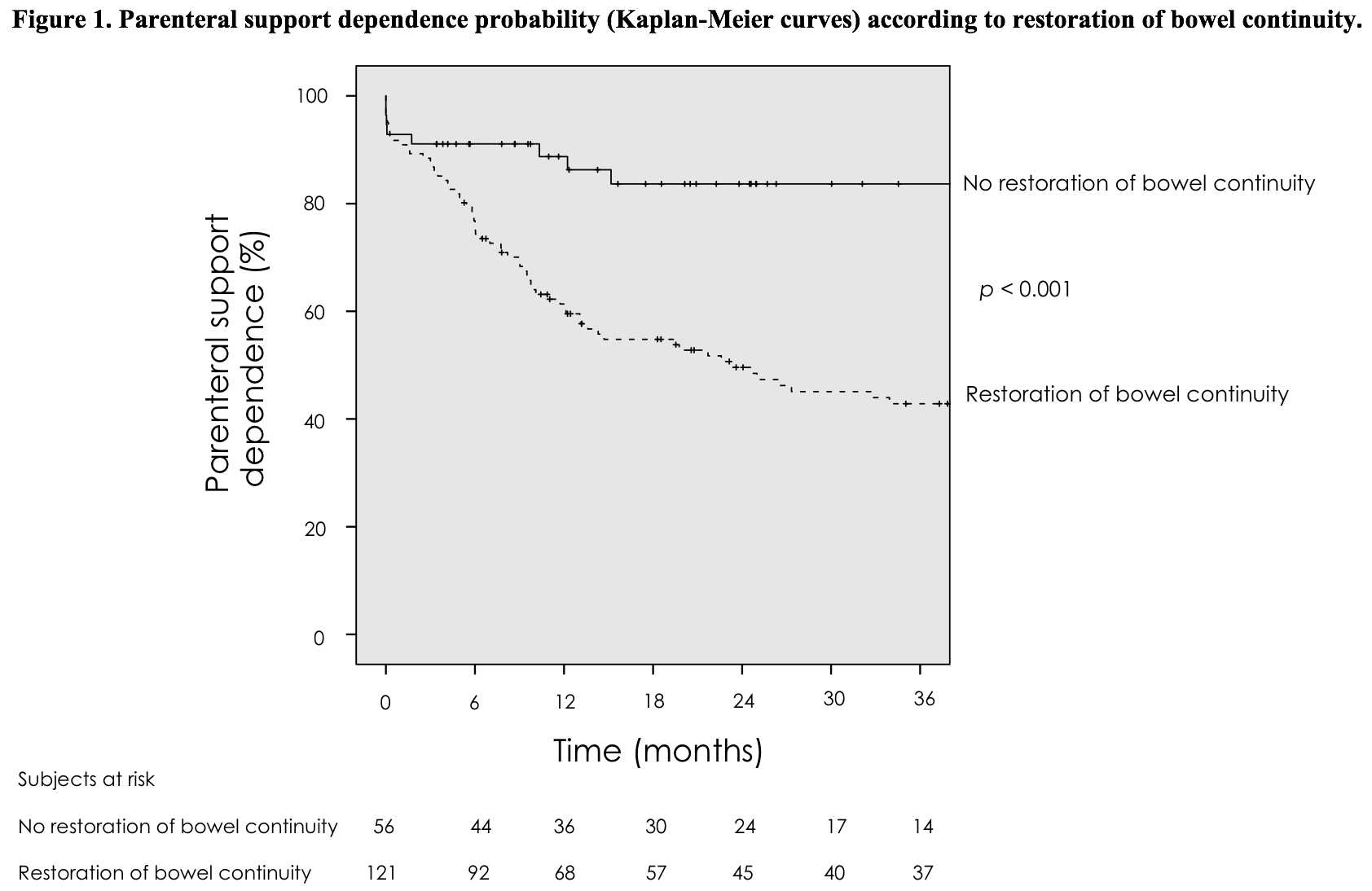
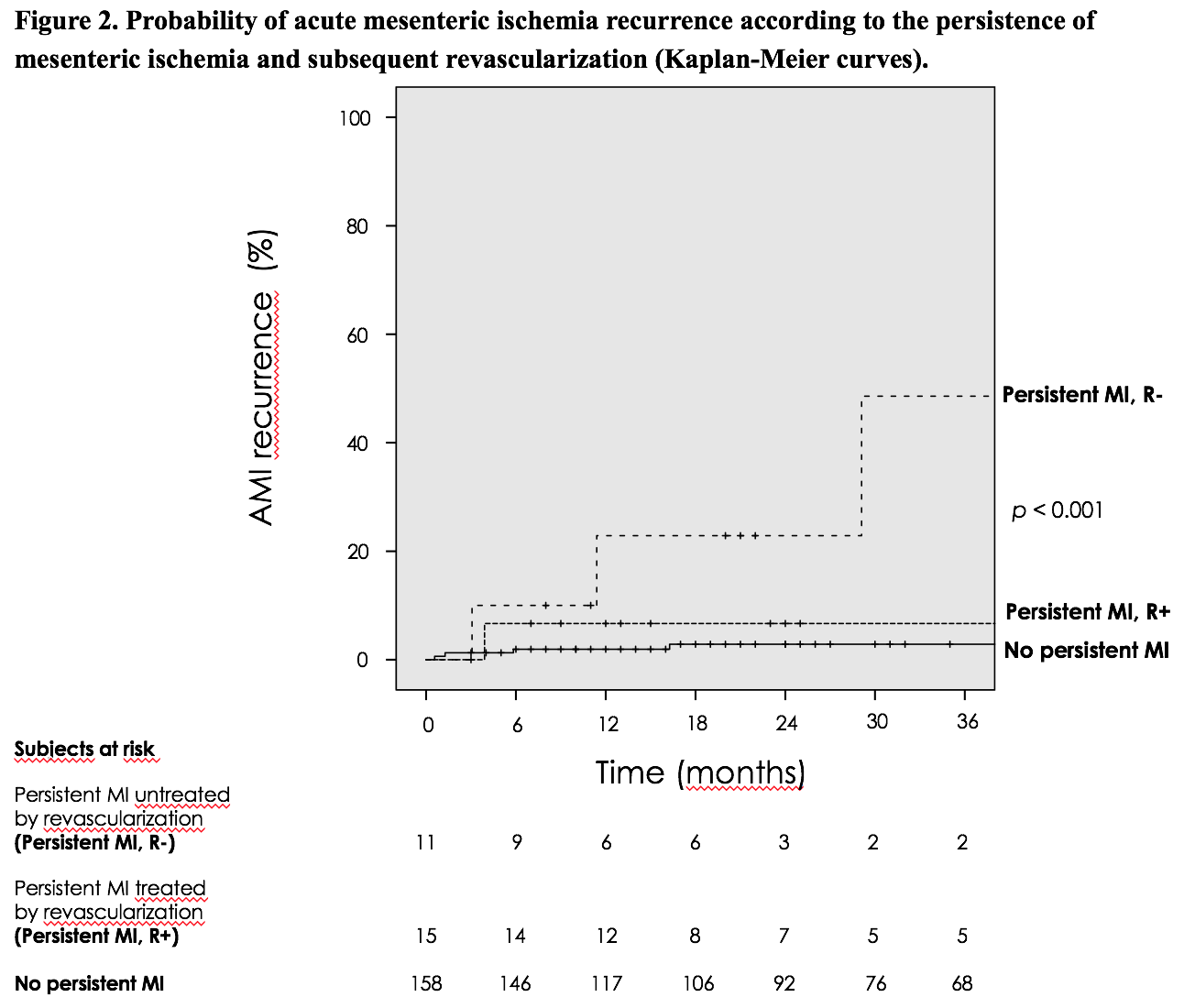
Results: We included 184 patients (median age 51) referred to our unit median 3 months after surgery for AMI. Upon diagnosis, AMI was the first ever reported cardiovascular event in 53% of patients and lactate plasma levels were within normal range in 49%. Early-stage AMI was misdiagnosed (median diagnosis delay: 2 days) and under-treated (revascularization rates: 15%) resulting in bowel resection and IF in all patients. After multidisciplinary (i.e.nutritional, vascular and digestive) rehabilitation, 3-year survival probability was 86%, with no AMI recurrence in 94%, no stoma in 70% and no PS dependence in 47% of patients. In multivariate analysis, initial revascularization [HR=2.4; 95%CI=1.1-5.2; p=0.02], remnant bowel length > 50cm [51-150cm: HR=3.8; 95%CI=1.8-8.0; >150cm: HR=9.7; 95%CI=3.9-23.8; p<0.001] and restoration of bowel continuity [HR=4.7; 95%CI=2.0-11.4; p=0.001] were predictors of long-term PS independence (Figure 1). We observed 11 cases (6%) of AMI recurrences median 11.4 months after the primary AMI episode. The probability of AMI recurrence was 3% in patients without persistent mesenteric ischemia (MI) and rose to 7% in patients with persistent MI treated by revascularization (unadjusted p=0.15) and 48% in patients with persistent MI left untreated by revascularization [adjusted p<0.001, HR=14.1 95%CI=3.9-51.7)] (Figure 2).
Conclusion: Surgical AMI patients initially presented at an early, potentially reversible but misdiagnosed and under-treated stage. Expert multidisciplinary rehabilitation, however, allowed high PS-free long-term survival. The utmost attention should be given to timely recognition, revascularization and expert care at both the acute and rehabilitation stages of AMI.
.jpg )