Background: Long-term parenteral nutrition(PN) is essential for the survival of children with intestinal failure(IF) but it contributes to morbidity & economic burden. We aimed to characterise the clinical & financial impact of long-term PN burden in the 1st 5 yrs of our intestinal rehabilitation program established in 2014 at a single-centre in Singapore.
Methods: A retrospective cohort review of children with IF who had long-term (>90 days) PN & transitioned to home-PN (HPN) from 2014 – 2018 was done. All complications related to long-term PN & the underlying gastrointestinal/surgical disorder were collected. Financial data was retrieved from the hospital’s business office. Costs were categorized into 1)PN-related, 2)underlying disease (UD)-related including investigations, surgery, intensive care, & complications from UD; or 3)unrelated. In Singapore, healthcare cost is borne by the patient, with varying proportion of government subsidy.
Results: 18 children (11 girls) with IF received long-term PN for median duration of 1.36(0.27-7.5) yrs. Aetiologies included necrotizing enterocolitis 50%, paediatric intestinal pseudo-obstruction 27%, congenital mucosal disorders 11%, malrotation 5.6% & inflammatory bowel disease 5.5%. The median age at PN-onset was 0.66(0.03-68) months and at HPN-onset was 2.19(0.63-7.26) years.11 patients received hospital-PN while 7 were transitioned to HPN. 64% achieved enteral autonomy after a median duration of 1.13(0.27-6.95) years of PN support. Central line-associated bloodstream-infections affected 77% of patients with an incidence rate of 4.6/1000 catheter-days. Other major complications were recurrent venous thrombosis 50% & intestinal failure-associated liver disease 38%. One patient died from sepsis at 6 months of age, no patient has undergone intestinal or liver transplantation.
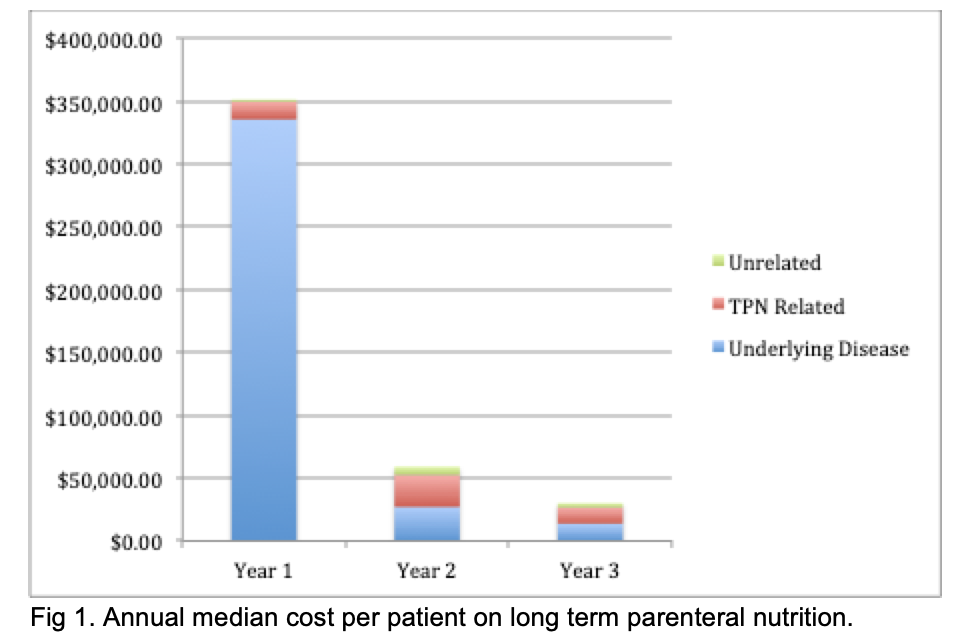
The overall median cost of managing children with IF for the 1st year was US$350,232.30/patient. It dropped to US$59,331.01 in the 2nd yr & US$30,149.91 in the 3rd yr. In the first yr, 95% of costs were UD-related while 5% were PN-related. Subsequently, the proportion spent on PN was 43% while costs due to UD dropped to 45% (Fig).
Conclusion: Long-term PN therapy, whilst an effective life-saving option for paediatric IF, incurs substantial financial burden to families and the healthcare system. These findings should form the basis of a cost-benefit analysis of initiating an intestinal/multi-visceral transplantation program for patients with irreversible IF.
.jpg )