Introduction: There is no centralized registered information regarding patients (pts) suffering from Short Bowel Syndrome (SBS) in Argentina. Estimations based on other countries epidemiology predict an incidence of 8-10 new adult pts/year. In order to compile this information, we started a prospective multicenter observational and epidemiological registry for adults with SBS, independent from the etiology and the treatment proposed. We aim to present the first report of the RESTORE project.
M-M: From 2015 to 2017, design, funding, Institutional Review Board and Ethical approvals were obtained. Since June 2017, 11 centers started activity. Data collection was made using case report forms; a monitor visited and supervised each center initiation and performance. The registered pts are followed at each center at weeks 4, 8, 12, 20 and 24, and yearly thereafter. Dead, intestinal adaptation and transplant have been considered as end-points of the study. The principal investigator developed a prospective database. Statistical analysis was done on SPSS v20.0.
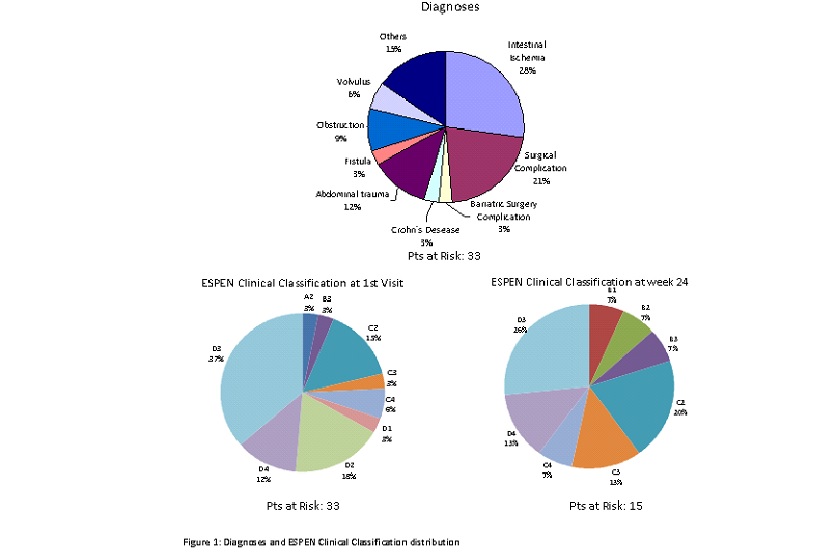
Results: 12 centers were initiated, 10 enrolled 42 pts; 33 pts were actively monitored and analyzed,12 pts completed 1 year of follow up (FU); 19 pts (57.6%) were female; mean age: 52.15 ± 15.4 years. Diagnoses in Figure 1. Mean intestinal length: 51.5 ± 42.4 cm. Anatomy type: T1: 22 pts; T2: 8 pts and T3: 3 pts; ileo-cecal valve was present in 11pts. Colon in 27 pts; Ostomies in 22 pts. Mean ostomy output: 1514 ± 1078 ml/day; Autologous GI tract Reconstruction Surgery (AGIRS) was done in 11 pts before enrollment. Meantime on parenteral nutrition (PN) before enrollment: 27.4 ± 37.18 months; PN and biochemical variables overtime are shown in Table 1; Espen Clinical Classification in Figure 1.
Treatments proposed at first visit: PN+ Medical Rehabilitation: 20 pts (60%), AGIRS: 4 pts (12%); post-surgical teduglutide (TED): 8 pts (24%); transplant: 1 pt (3%); at the end of FU: 1pt was lost of FU; 4 pts adapted with AGIRS alone, or in combination with TED. One pt was transplanted and another pt. listed due to liver disease. The overall actuarial survival is 87%; sepsis was the main cause of death (3/4 pts).
Conclusions: Although this report still has a limited number of centers, it has registered more SBS adult patients than expected according to theoretical estimations; reinforcing the importance of having registries to understand the behavior of SBS patients overtime and their outcome.
.jpg )