Objective: Visceral transplantation (VT) is indicated in patients who have failed intestinal rehabilitation and have complications related to parenteral therapy. VT outcomes from an academic center over a 20-year period were studied.
Methods: Between 1/1996 and 12/2015, 212 pediatric patients underwent 235 VT. There were 23 re-transplants. Index VT included isolated small bowel (SB n=90); liver, pancreas, small bowel (L+SB n=86); liver, stomach, pancreas, small bowel (multivisceral MVT n= 28); or stomach, pancreas, small bowel (modified multivisceral MMVT n=7) with or without colon. M/F ratio was 125/87. Immunosuppression was antibody induction, tacrolimus and steroids. VT indications were gastroschisis (n=52), intestinal atresia (n=21), volvulus (n=49), necrotizing enterocolitis (n=24), pseudo-obstruction (n=27), Hirschsprung’s disease (n=17), microvillous inclusion disease (n=12), others (n=11).
Results: 140 patients are alive between 2 and 23 years after transplant (mean 12.8 years). 31 of these underwent allograft enterectomy for rejection (n=26), technical (n=3), primary nonfunction (n=1), PTLD (n=1), and are on parenteral nutrition. 11 in this group were re-transplanted.
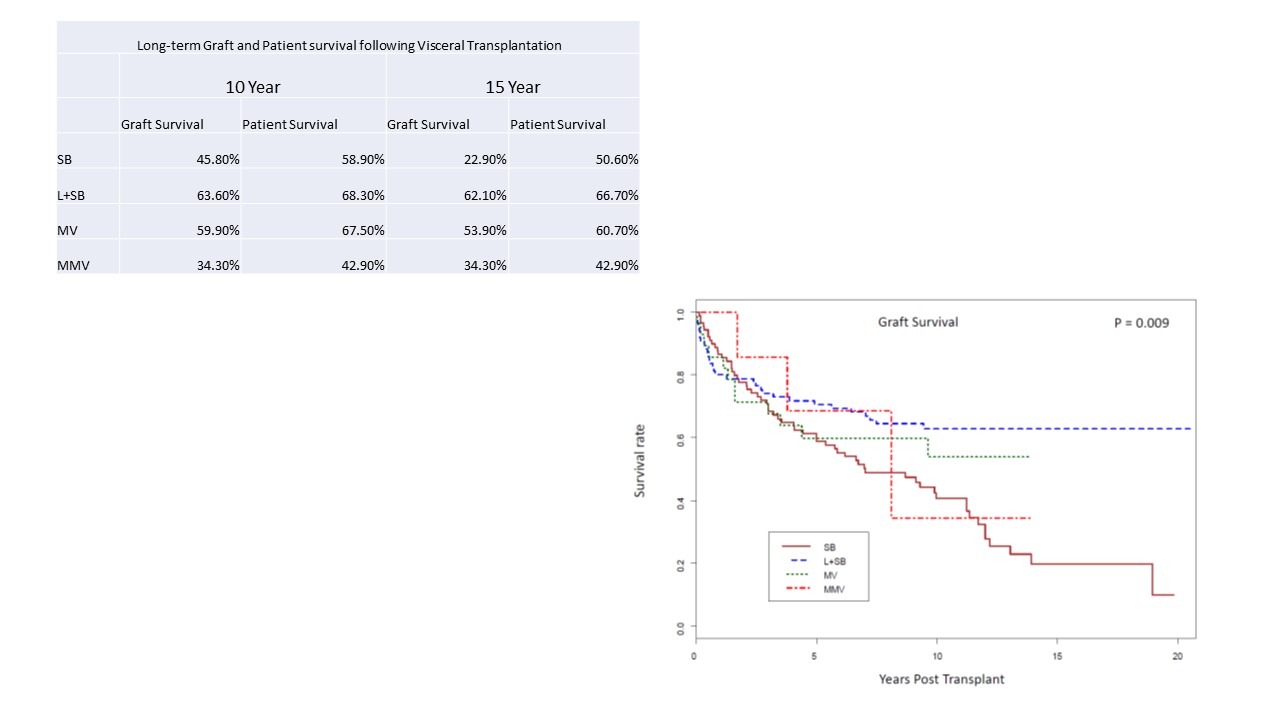
77 patients died between 4 days and 20.5 years following visceral transplant (mean 44.5 months). Infection and multisystem organ failure was the leading cause of death (n=26, 31%). Maximum 10 and 15-year graft and patient survival were observed in LB recipients confirming liver’s protective role in sustaining small bowel grafts (table and graph; p=0.009).
Conclusions: Visceral transplantation is a viable option for patients with intestinal failure and offers long-term benefit and freedom from parenteral nutrition. Infection continues to be a major factor responsible for graft loss. With careful patient selection and comprehensive management by multidisciplinary team prolonged nutritional autonomy can be restored.
.jpg )