Introduction: Short Bowel Syndrome (SBS) can occur at any age, but the majority of paediatric cases result following bowel resection in infants with congenital abnormalities or those developing necrotising enterocolitis (NEC). Parenteral nutrition (PN) is needed during bowel adaptation and if required for an extended period treatment is continued at home (HPN). We describe our experience of HPN patient demographics and outcome in three time periods with different approaches to patient care.
Methods: Inclusion: Infants with neonatal SBS receiving HPN 1987-2015. Exclusion:1) patients acquiring SBS outside the neonatal period 2) patients starting HPN in other units 3) patients born 2016-2018 with outcome still undetermined. Data was collected from dietetic records and HPN database and included cause of SBS, time to discharge and outcome. In patients weaned from PN time to full enteral nutrition (EN) was recorded. Data from three time periods 1987-1996 (Cohort 1), 1997-2006 (Cohort 2) and 2007-2015 (Cohort 3) were compared.
Results:
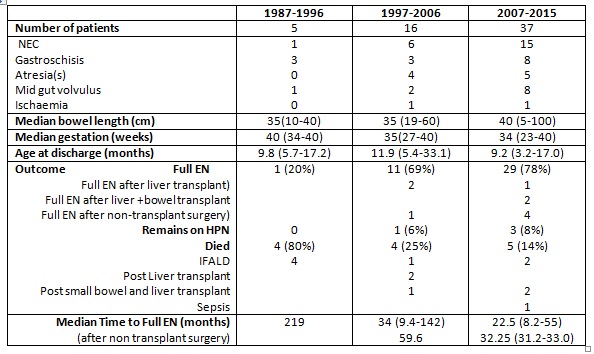
142 patients have been managed on HPN since 1987. SBS was the indication in 51% patients. Patient numbers increased, the proportion with NEC rising significantly: Cohort 1 20% patients, Cohort 2 38% and Cohort 3 41%. There was no significant difference in median bowel length. Median age at discharge was lowest in Cohort 3. Survival was 20% Cohort 1, 75% Cohort 2 and 86% Cohort 3. 80% patients in Cohort 1 died of intestinal failure associated liver disease (IFALD) reducing to 6% in Cohort 2 and 3. Median time to full EN was shortest in Cohort 3 and was not improved by non-transplant surgery.
Conclusion: Data shows an increase in the number of infants with SBS requiring HPN, mainly due to a rise in preterm infants with NEC. Cohort 3 shows markedly improved outcomes: 78% patients achieved full EN in median time 22.5 months. Advances in transplantation have contributed to reduction in death from IFALD but 75% deaths in cohort 2 (n=3) and 40% deaths in Cohort 3 (n=2) occurred post-transplant. Long-term PN remains the treatment of choice in children unable to wean from PN. Successful management of infants receiving HPN requires skills of a multidisciplinary nutrition team: aggressive use of enteral nutrition, early discharge, improved management of catheter sepsis, advances in transplantation all impact on survival of infants with SBS requiring HPN.
.jpg )