Introduction: Tissue-resident memory (TRM) T cells, long-lived effector T cells in tissue that do not recirculate, are critical in inflammatory, infectious, and neoplastic conditions1. However, the study of human TRM cells has been hampered by an inability to prove long-term tissue residency. We hypothesised that intestinal transplantation could present an opportunity to study long-lived donor-derived TRM cell populations.
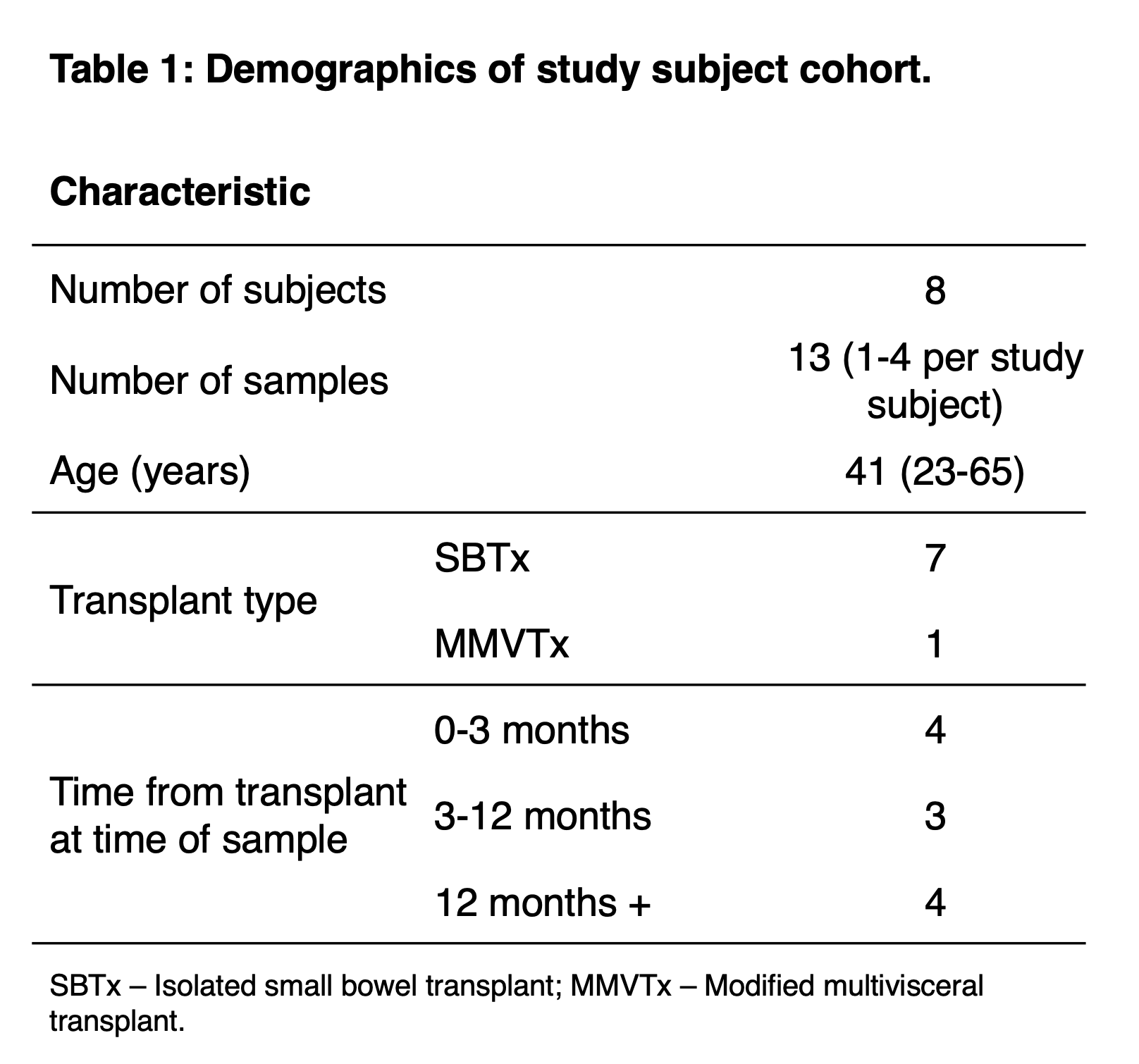
Methods: Adult intestinal transplantation recipients were identified via longitudinal cohort studies at Oxford University Hospitals NHS Foundation Trust. Thirteen samples of intestinal graft biopsies were obtained from eight patients (Table 1).
Donor- and recipient-derived T cells in intestinal transplant mucosa were identified using flow cytometry and antibodies to discordant HLA Class I proteins (Fig 1A)2. Proposed residency markers CD69 and αE integrin (CD103) were included in the panel. Fluorescence-activated cell sorting was used to sort donor- and recipient- derived intestinal T cells for 5’ single-cell RNA sequencing using the 10X Genomics platform.
Results: The proportion of donor-derived T cells was negatively correlated with time post-transplant, and was highly variable between subjects, with some subjects maintaining significant donor-derived populations up to 5 years post-transplant (Fig 1B). Donor-derived T cells uniformly expressed CD69 (>99%), and CD103 was highly expressed (84%), with increased expression at late times (Fig 1C).
Single-cell RNA sequencing was performed on cells sorted from a single healthy subject 1 year post-transplantation. Data from 974 cells were of sufficient quality for analysis. Analysis of gene expression revealed conventional CD4 T cells, CD4 TREGS, and 2 distinguishable CD8 T cell populations within the graft-resident donor-derived cells (Fig1D). The CD8 clusters differed in expression of key residency (CD103) and functional markers (GzmB and HLA class II) (Fig 1E).
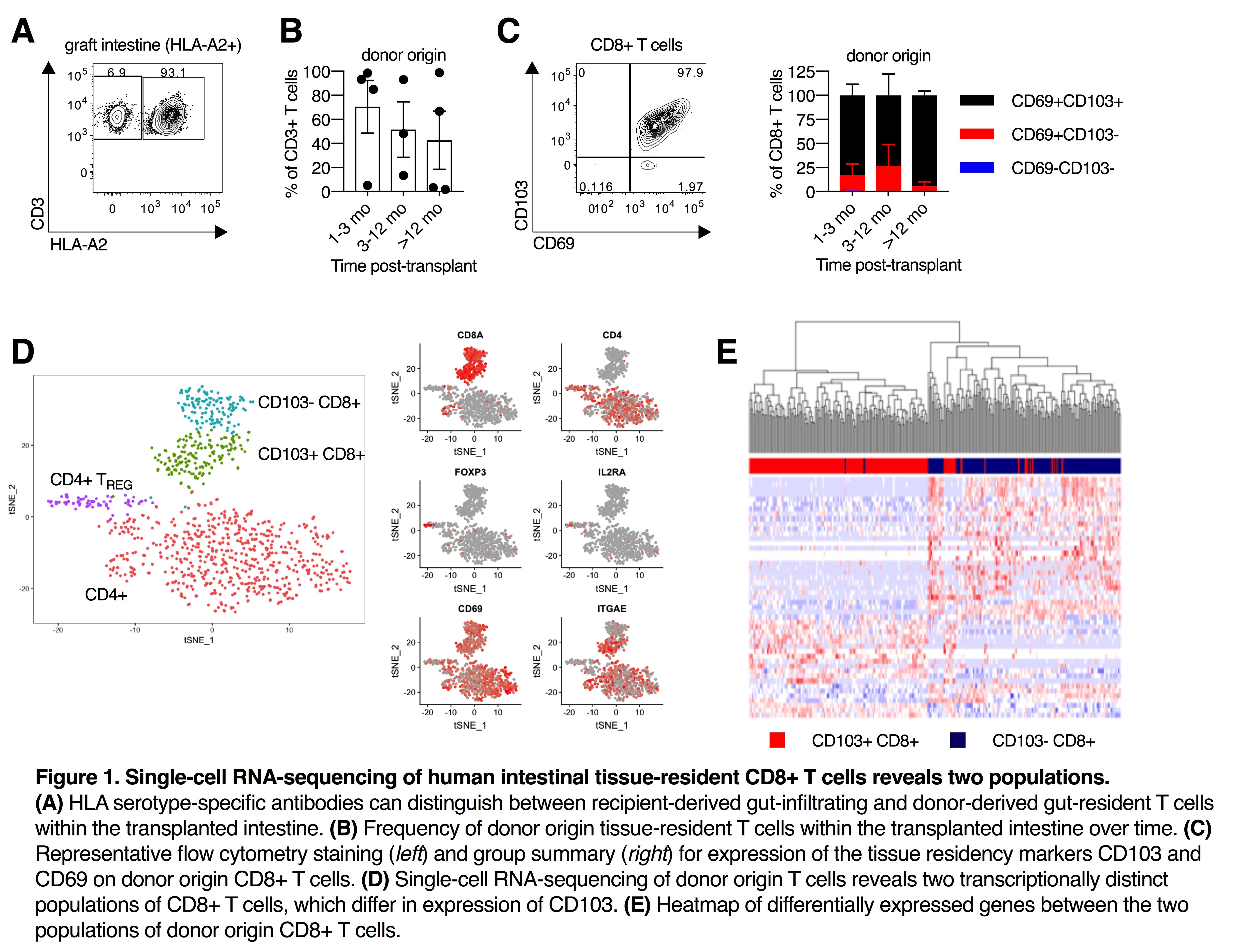
Conclusion: Donor-derived TRM cells can persist in the graft for at least 5 years post-transplant, with highly variable dynamics between patients. Single-cell transcriptomic profiling and flow cytometry indicates two transcriptionally and phenotypically distinct CD8 TRM populations within the human intestine. Further study of the regulation, differentiation, and biology of these populations is warranted, as well as their role in intestinal transplantation.
1. Mueller & Mackay (2015) Nat Rev Immunol
2. Zuber J. et al. (2016) Sci Immunol
.jpg )